Retina Specialist London
Mr James Neffendorf, Consultant Retinal Surgeon, providing expert care for all retinal conditions.
Excellent
4.96 out of 5
What is the Retina?
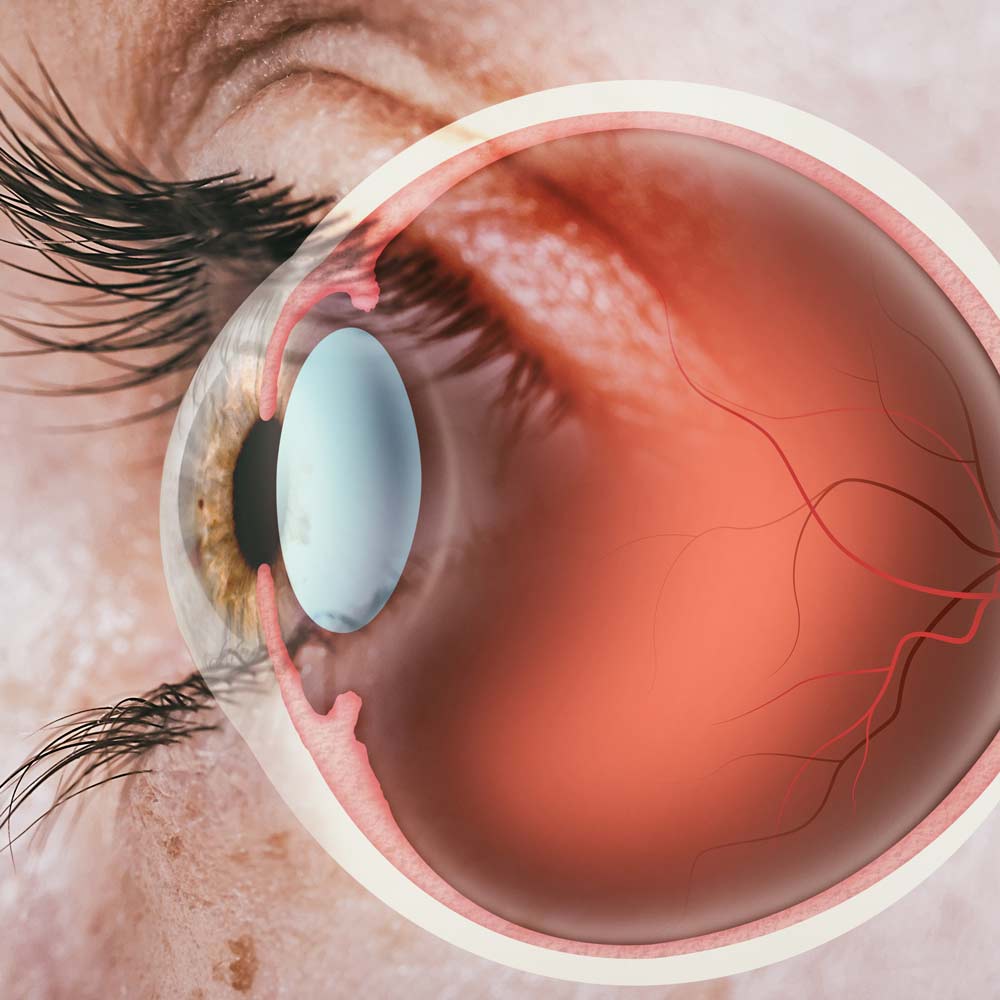
The retina is a thin structure which lines the inside of the eyeball. It is the layer which enables you to see, akin to the film of the camera. It is a complex structure, made up of many layers and millions of cells. Despite this, it only measures approximately 0.5mm in thickness. A healthy functioning retina is crucial to ensuring you can see clearly.
The retina captures light that is focused upon it. The centre of the eyeball is called the vitreous cavity, and this is filled by a gel-like structure made up of water, hyaluronic acid and collagen.
Retina and Vitreous Conditions
Many conditions can affect the retina and vitreous. These range from common issues such as floaters to sight-threatening emergencies such as retinal detachment.
The retina can also be affected by systemic conditions such as diabetes and high blood pressure. In some cases, examination of the retina can identify these conditions before they have been formally diagnosed, which demonstrates the importance of a regular eye check-up.
There are also some conditions of the retina and vitreous which do not present with any symptoms in their early stages and therefore regular review by an expert can help you identify, monitor and treat a problem early.
When to See a Retina Specialist?
You should see a retina specialist if you develop symptoms that signal a retinal problem. Early identification of symptoms and an early diagnosis can make a significant difference to the long-term visual outcome.
Why Timing Matters
Early identification of symptoms is important because most conditions of the retina and vitreous which require laser, injections or surgery have a far better long-term visual outcome if they are treated early, rather than late.
If you experience any of these symptoms, an assessment by Mr Neffendorf can help identify the underlying cause and guide treatment.
Why Choose Mr Neffendorf
Choosing the right specialist can feel overwhelming. Mr Neffendorf is one of a small number of ophthalmologists who is highly specialised at looking after patients with diseases or problems of the retina and vitreous.
Consultant Ophthalmologist at King’s College Hospital NHS Foundation Trust
Fellowship-trained in Vitreoretinal Surgery at St Thomas’ Hospital, London
Known for his communication skills, patient-centred approach and taking time to explain conditions and treatment clearly
Published 39 scientific papers and presented at 40 international and national meetings
Recipient of multiple awards, including recognition from the American Academy of Ophthalmology and EURetina
Examiner for the Royal College of Ophthalmologists and reviewer for multiple leading peer-reviewed journals
Symptoms
There are many symptoms that might indicate problems in the retina and vitreous.
Symptoms that may indicate a retinal or vitreous problem:
A curtain or shadow across your vision
Flashes of light in your field of view
New or worsening floaters
Areas of lost vision (blind spots)
Distorted central vision
General vision changes, becoming reduced or cloudy
If you experience any of these symptoms, an assessment by Mr Neffendorf can help identify the underlying cause and guide treatment.
There are also some conditions of the retina and vitreous which do not present with any symptoms in their early stages, and therefore regular review by an expert can help you identify, monitor and treat a problem early.
Conditions Treated
Specialist care for conditions affecting the retina and vitreous.
Vitreous Floaters

In many cases, floaters are not indicative of a serious underlying problem. In this scenario, they can be annoying as they might interfere with your vision, but they do not cause harm and often will become less noticeable with time. Laser or surgery can be performed for persistent troublesome floaters.
Epiretinal Membrane (ERM)

Macular Holes (MH)

Posterior Vitreous Detachment (PVD)

The main symptoms of a PVD are flashing lights and/or floaters. If you develop these, it is important to be examined by a retina specialist within 24-48 hours. Approximately 10% of patients who develop a PVD have a retinal tear which requires urgent laser or cryotherapy treatment to reduce the chance of a retinal detachment (see below) developing. Untreated retinal tears carry a significant risk of a retinal detachment which is a sight threatening emergency.
Retinal Tear

Retinal Detachment

It is more common in short-sighted people (myopia), those who have previously had cataract surgery, and those with a history of trauma to the eye. There are other forms of retinal detachment without retinal tears due to traction on the retina (e.g. in diabetic patients) or excessive fluid production under the retina. The symptoms that might indicate a retinal detachment has occurred are flashing lights, floaters and a curtain/shadow in the vision. Some patients do not present with all symptoms, and sometimes a retinal detachment can be asymptomatic (have no symptoms). The majority of retinal detachments progress and with time will cause a rapidly progressing shadow of vision loss that eventually affects the central vision and ultimately entire vision of the eye. It is therefore important that if you develop any of these symptoms you are seen urgently by a vitreoretinal surgeon, such as Mr. Neffendorf.
The vast majority of retinal detachments need to be repaired urgently. Delay in surgery can result in severe loss of sight and blindness. The earlier a retinal detachment surgical repair is performed, the more likely you are to preserve your sight. There are different ways to repair a retinal detachment, which Mr. Neffendorf will discuss with you in a consultation. Further information is available in the Patient Information Leaflet in the Patient Info. section.